The Brain and Stroke
- Info OT and Me
- Dec 20, 2022
- 7 min read
Updated: Jan 23, 2023
What is a Stroke?
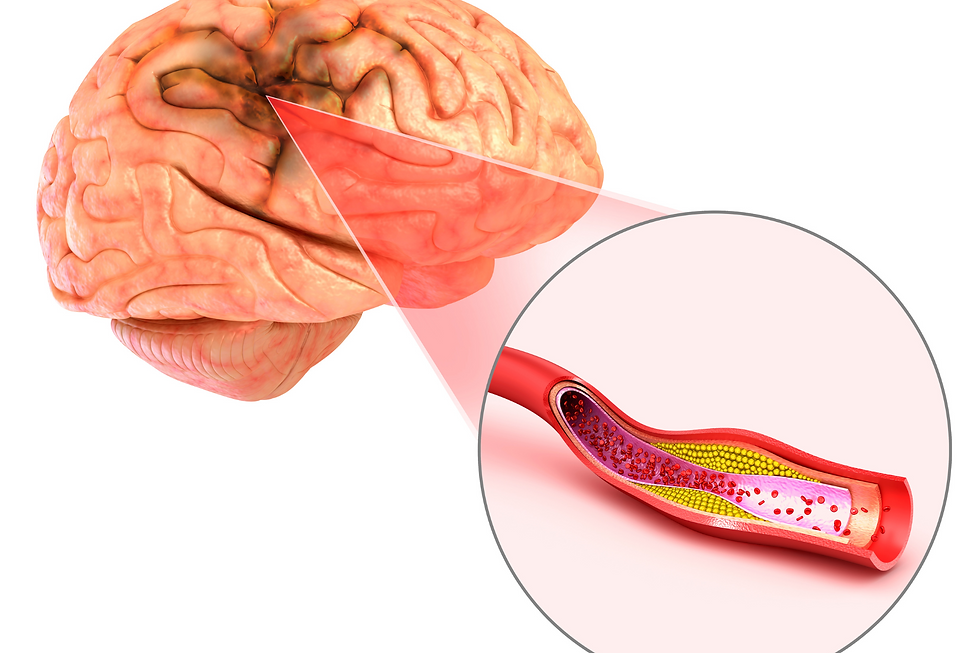
A stroke, also known as a cerebral vascular accident, is a medical condition that occurs when the blood supply to a part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. This deprivation can damage or destroy brain cells.
There are two main types of stroke: ischemic stroke and hemorrhagic stroke. An ischemic stroke occurs when a blood vessel that carries oxygen and nutrients to the brain becomes blocked, usually by a blood clot. A hemorrhagic stroke occurs when a blood vessel in the brain ruptures and bleeds into the surrounding brain tissue.
Strokes are medical emergencies because they can cause severe and permanent brain damage, significantly impacting a person's quality of life. The brain is an essential organ that controls many of the body's functions, including movement, sensation, and cognitive abilities such as memory, speech, and decision-making. When a stroke occurs, the lack of blood flow to a part of the brain can damage or destroy brain cells, leading to various symptoms, such as paralysis, difficulty speaking, and problems with memory and other cognitive functions.
What areas of the brain are affected by stroke?
The areas of the brain commonly affected by a stroke depend on the location of the disrupted blood vessel. Different parts of the brain control different functions, so the symptoms of a stroke can vary depending on which part of the brain is affected.
For example, if a stroke affects the brainstem, the lower part of the brain that connects to the spinal cord, it can cause problems with breathing, heart rate, and blood pressure problems. A stroke in the cerebellum, which is the part of the brain that controls balance and coordination, can cause difficulty with balance and coordination and problems with movement and speech.
About 878,000 Canadian adults aged 20+ have experienced a stroke - Government of Canada
A stroke in the cerebral cortex, which is the outer layer of the brain that is responsible for many of the brain's higher functions, such as thinking, decision-making, and perception, can cause a variety of symptoms, including paralysis, difficulty speaking, and problems with memory and other cognitive functions.
If a stroke is not treated promptly, the damage to the brain can be permanent, resulting in long-term disability or even death. It is essential to seek medical attention as soon as possible if you or someone you know experiences symptoms of a stroke. The sooner treatment is received, the greater the chances of minimizing the damage caused by the stroke and improving the chances of a full recovery.
How to tell if someone is having a stroke?
Here are some common signs and symptoms of a stroke:
Sudden weakness or numbness on one side of the body: This can include weakness in the arm, leg, or face or a feeling of numbness in the face, arm, or leg.
Difficulty speaking or understanding speech: The person may have trouble speaking or understanding what others are saying or may slur their words.
Difficulty seeing in one or both eyes: The person may experience sudden vision loss in one or both eyes or see double.
Dizziness or loss of balance: The person may feel dizzy or unsteady or have trouble walking or standing.
Severe headache: The person may experience a sudden, severe headache different from usual.
If you notice any of these symptoms in yourself or someone else, it is important to call emergency services immediately. The acronym FAST can help you remember the most common signs of a stroke:

F: Face drooping.
A: Arm weakness.
S: Speech difficulty.
T: Time to call emergency services.
If you see any of these signs, even if they go away quickly, it is crucial to seek medical attention immediately.
What are some common risks factors for strokes?
Several risk factors can increase a person's likelihood of having a stroke. Some risk factors are non-modifiable, meaning they cannot be changed, while others are modifiable, meaning they can be changed or controlled through lifestyle changes or medical treatment.
Non-modifiable risk factors for stroke include:
Age: The risk of stroke increases with age.
Gender: Men are more likely to have a stroke than women.
Family history: If a close relative has had a stroke, a person may have an increased risk of stroke.
Modifiable risk factors for stroke include:
High blood pressure: High blood pressure is a leading cause of stroke.
High cholesterol: High cholesterol levels in the blood can increase the risk of stroke.
Smoking: Smoking increases the risk of stroke by damaging the blood vessels and increasing the likelihood of blood clots.
Diabetes: People with diabetes have an increased risk of stroke due to the damage that high blood sugar levels can cause to the blood vessels.
Obesity: Being overweight or obese increases the risk of stroke due to the strain it places on the heart and blood vessels.
Lack of physical activity: A sedentary lifestyle can increase the risk of stroke.
Alcohol consumption: Excessive alcohol consumption can increase the risk of stroke.
Managing these modifiable risk factors through lifestyle changes, such as maintaining a healthy diet and exercise routine, quitting smoking, and controlling diabetes and high blood pressure, can help reduce stroke risk. It is also important to follow the advice of a healthcare provider to manage any medical conditions and reduce the risk of stroke.
1/4 of Canadian Living with stroke are under age 65 -Government of Canada
Stroke Treatment and Recovery Management
Several treatments are available for stroke, depending on the type and severity, the person's age and overall health. Stroke treatment typically involves a combination of medications, rehabilitation, and lifestyle changes.
Medications:
Thrombolytic drugs are used to dissolve blood clots that cause ischemic strokes. They must be given as soon as possible after the stroke to be effective.
Antiplatelet drugs are used to prevent blood clots from forming and can be given to people who have had a stroke to prevent future strokes.
Blood pressure-lowering medications are used to lower high blood pressure, a significant risk factor for stroke.
Cholesterol-lowering medications are used to lower high cholesterol levels, which can increase the risk of stroke.
Rehabilitation:
Physical therapy can help improve mobility and function after a stroke.
Occupational therapy can help with activities of daily living, such as dressing, bathing, and eating.
Speech therapy can help with speech and language problems that may occur after a stroke.

Lifestyle changes:
Diet: A healthy diet low in salt, saturated fat, and cholesterol can help reduce the risk of stroke.
Exercise: Regular physical activity can help lower blood pressure and improve cardiovascular health, reducing the risk of stroke.
Smoking cessation: Quitting smoking can significantly reduce the risk of stroke.
Alcohol consumption: Limiting alcohol consumption can also help reduce stroke risk.
Working with a healthcare team, including a doctor, nurse, and other healthcare professionals, is crucial to determine the most appropriate treatment plan for a stroke. Stroke treatment should be tailored to the individual's specific needs and may involve a combination of medications, rehabilitation, and lifestyle changes.
How does Occupational Therapy help?
Occupational therapy is crucial in rehabilitating people who have had a stroke. Occupational therapy focuses on helping individuals to regain the skills and abilities needed to perform activities of daily living (ADLs) and to return to their daily routines as independently as possible.
After a stroke, a person may experience physical or cognitive impairments that affect their ability to perform ADLs, such as bathing, dressing, and eating. Occupational therapy can help improve or restore these skills through various techniques and strategies.
Occupational therapists may use task-specific training, which involves practicing a specific activity repeatedly to improve the person's ability to perform it. They may also use adaptive equipment, such as modified utensils or dressing aids, to help the person perform ADLs more easily.
In addition to helping with ADLs, occupational therapists may also work with individuals to develop strategies for managing their physical and cognitive impairments, such as memory problems or difficulty with decision-making. They also help individuals set goals and develop a plan to achieve them.
Overall, the goal of occupational therapy in stroke rehabilitation is to help individuals regain the skills and abilities needed to live as independently as possible and to return to their daily routines and activities. Working with an occupational therapist can be an essential part of the recovery process after a stroke.
Stroke risk rises rapidly after age 55 - Government of Canada
What are some Occupational Therapy specific treatments?
Occupational therapists use a variety of treatments to help individuals recover from a stroke. The specific treatments used will depend on the individual's needs and goals and the severity and type of impairments they are experiencing. Here are some common treatments that occupational therapists may use for stroke recovery patients:
Task-specific training: This involves practicing a specific activity repeatedly to improve the person's ability to perform it. For example, an occupational therapist may work with patients to practice writing or grasping objects to improve their fine motor skills.
Adaptive equipment: Occupational therapists may use adaptive equipment, such as modified utensils or dressing aids, to help the person perform activities of daily living (ADLs) more easily.
Cognitive rehabilitation: This may include exercises to improve memory, attention, and other cognitive skills that may have been affected by the stroke.
Sensory reeducation: This may involve activities to help the person process and interpret sensory information, such as touch or sight, that may have been affected by the stroke.
Assistive technology: Occupational therapists may recommend assistive technology, such as voice-activated devices or computer software, to help the person communicate or perform tasks more efficiently.
Environmental modification: Occupational therapists may suggest changes to the person's home or work environment to make it more accessible and easier to navigate.
Education: Occupational therapists may educate the person and their family about stroke recovery and how to manage impairments and disabilities.
Occupational therapists work with individuals to develop a treatment plan tailored to their specific needs and goals.

How long does it take to recover from a stroke?
The length of time it takes to recover from a stroke can vary greatly depending on the severity of the stroke, the location of the blood flow disruption, the person's age and overall health, and their level of motivation for recovery. Some people may recover within a few weeks or months, while others may have long-term or permanent impairments that require ongoing rehabilitation and support.
In the early stages of stroke recovery, the person may need to stay in the hospital for medical treatment and rehabilitation. After being discharged from the hospital, the person may continue to receive rehabilitation services on an outpatient basis or at home. Rehabilitation may include physical, occupational, speech, and other therapies to help the person regain function and independence.
The length of time it takes to recover from a stroke can also depend on the person's ability to adhere to their treatment plan and make lifestyle changes that can help to prevent future strokes. This may include following a healthy diet, exercising regularly, quitting smoking, and controlling any medical conditions, such as high blood pressure or diabetes.
The recovery process after a stroke is often long and challenging. Still, with the proper treatment and support, many people can make significant progress and improve their quality of life.
Download the Government of Canada Stroke Infographic below...
References:
Canada, P. H. A. of. (2019, December 9). Government of Canada. , 2017 - Canada.ca. Retrieved December 20, 2022, from https://www.canada.ca/en/public-health/services/publications/diseases-conditions/stroke-canada-fact-sheet.html
Khaku AS, Tadi P. Cerebrovascular Disease. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430927/
Public Health Agency of Canada. (n.d.). Stroke in Canada - Canada.ca. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/stroke-in-canada.html



Comments